Ready to enroll in a health insurance plan? Shop Now
Referral Authorization Forms | Ambetter from SilverSummit HealthPlan
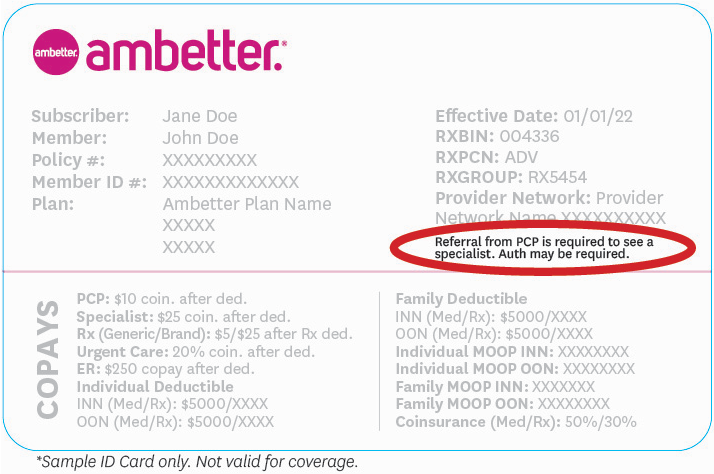
Referral and Authorization Information
-
 Ambetter Essential, Balanced and Secure Care Plans
Ambetter Essential, Balanced and Secure Care Plans -
 Ambetter Value Plans
Ambetter Value Plans
Ambetter Essential, Balanced and Secure Care Plans
Referrals
If you have a specific medical problem, condition, injury or disease, you may need to see a specialist. A specialist is a provider who is trained in a specific area of healthcare. Talk to your Primary Care Provider (PCP) first. He/she will refer you to a specialist for care if necessary. Do not go to a specialist without being referred by your PCP. The specialist may not see you without this referral.
It is also important you verify the specialist you are referred to is in the Ambetter from SilverSummit Healthplan network, so you don’t get billed for something you weren’t expecting.
Please note, there are some services that you may go directly to a specialist for without a referral. For example, you do not need a referral from your PCP for treatment from an in-network obstetrician or gynecologist. For a full listing of these services, please refer to your Evidence of Coverage - you can find it on your online member account at Ambetter.SilverSummitHealthPlan.com.
If you need care that your PCP cannot provide, he/she can recommend a specialist provider. Paper referrals are not required.
The following are services that may require a referral from your PCP:
- Specialist services, including standing or ongoing referrals to a specific provider
- Diagnostic tests (X-ray and lab)
- High tech imaging (CT scans, MRIs, PET scans, etc.)*
- Planned inpatient admission*
- Clinic services
- Renal dialysis (kidney disease)*
- Durable Medical Equipment (DME)*
- Home healthcare*
*Services above marked with an asterisk require prior authorization through Ambetter from SilverSummit Healthplan before receiving the service.
Prior Authorization for Services
Sometimes, we need to approve medical services before you receive them. This process is known as prior authorization. Prior authorization means that we have pre-approved a medical service.
To see if a service requires authorization, check with your Primary Care Provider (PCP), the ordering provider or Member Services. When we receive your prior authorization request, our nurses and doctors will review it. We will let you and your doctor know if the service is approved or denied.
Information about the review process, including the timeframes for making a decision and notifying you and your provider of the decision, is located in the Utilization Review section of your Member Handbook.
Failure to obtain prior authorization may result in a denied claim(s). To see a full listing of procedures and services that require PRIOR AUTHORIZATION, please log in to your secure member account to view your Schedule of Benefits.
The following services require the member’s provider to contact Ambetter from SilverSummit Healthplan for prior approval:
THE FOLLOWING LIST IS NOT ALL-INCLUSIVE
Ancillary Services
- Air ambulance transport
- Durable Medical Equipment (DME)
- Home health care services
- Hospice
- Furnished medical supplies
- Orthotics/prosthetics
- Genetic testing
- Quantitative urine drug screen
Procedures/Services
- Reconstructive Surgery
- Experimental or investigational
- High Tech Imaging administered by NIA (CT, MRI, PET)
- Submit requests to RadMD.com
- Pain management
- Cardiac and respiratory therapy
Inpatient Admissions
- All inpatient admissions (within 1 business day of admission)
- Observation stays exceeding 48 hours
- Notification is required within one (1) business day if admitted
- Transplants (not including evaluations
- Urgent/emergent admissions
- Partial inpatient, PRTF, and/or intensive outpatient programs
- All elective/scheduled admission notifications requested at least five (5) days prior to the scheduled date of admit including but not limited to:
- Medical admissions
- Surgical admissions
- Hospice care
- Rehabilitation facilities
Out-of-Network Services: All out-of-network services and providers require prior authorization, excluding emergency services.
You can also call your PCP or Ambetter from SilverSummit Healthplan Member Services with questions.
All out-of-network services require prior authorization, excluding emergency room (ER) services.
Ambetter Value Plan
Your Ambetter Value plan requires a referral from your Primary Care Provider (PCP) before you can see most specialists. Your claim will not be covered without a referral.
Here’s what you need to do:
1. Select Your PCP
If you haven’t already, select a PCP. You can view a list of recommended PCPs and select your PCP on Find a Doc.
2. Meet With Your PCP
Your PCP will help coordinate all your health care services and provide any necessary referrals. During your PCP visit you should discuss your goals, follow up with your Care Team, and obtain any necessary referrals.
Important!
- If you have an appointment already scheduled with a specialist, you will need to contact your PCP first. You will need to obtain a referral prior to the specialist visit.
- If you do not have a referral from your PCP, your specialist visit will not be covered. The claim will be denied, and it won’t be paid.
3. Schedule specialist visit
Members can see any in-network specialist with a referral.
Referrals are NOT required for the following services:
- Emergency services
- Urgent care services
- Mental health, behavioral health, and substance abuse services
- Obstetrical and gynecological care
Referral FAQs
Medical referrals are required to see a specialist if it's outside of the Primary Care Physicians' scope. Members must obtain a referral before consulting with an in-network specialist if they are a Value plan member.
Only your PCP may provide a referral for specialist care.
The claim will be denied.
No. Your PCP will need to submit a new referral if they determine additional specialist care is necessary.
No. If treatment is needed that may require Prior Authorization, the provider/specialist will need to follow the Prior Authorization process.
If the specialist feels that additional visits are needed beyond those requested by your PCP, a new referral will need to be submitted by your PCP.
You can seek a second opinion with another PCP in your Primary Provider Group.
Please allow seven (7) to ten (10) business days for the referral to be loaded on the member secure portal. You will then be able to view and print any referrals from your secure portal. You can also request a copy from your PCP.
If you are looking for a referral for a service that is not ‘on file' or in the system, this means your PCP has not submitted the referral. You will need to check with your PCP to ask for the referral to be submitted.
The following specialties do not require referral from your PCP. Services performed by these specialists may still require prior authorization.
- Urgent Care
- Emergency Care
- OBGYN
- Radiology/Imaging
- Anesthesia
- Mental Health
- Behavioral Health
- Substance Abuse Services
- Labs
Ambetter from SilverSummit Healthplan is underwritten by SilverSummit Healthplan, Inc., which is a Qualified Health Plan issuer in the Health Insurance Marketplace. This is a solicitation for insurance. © 2024 SilverSummit Healthplan, Inc. All rights reserved.
